Current Personnel
Karen Joos, MD, PhD, FARVO Joseph and Barbara Ellis Professor in Ophthalmology, Professor of Biomedical Engineering, Chief of the Glaucoma Division
Ratna Prasad, PhD, Senior Research Associate
Jin Hui Shen, Ph.D., Research Associate Professor (deceased)
Overview
The Joos research program is divided into two programs. The first investigates the development of ophthalmic surgical procedures using optical coherence tomography (OCT) and robotic surgery, and the second seeks to investigate the role of molecular and genetic components in glaucoma.
I. The first program is designed to develop and test intraocular surgical techniques with optical coherence tomography (OCT) including a 25-gauge intraocular OCT probe. Currently, in collaboration with Nabil Simaan, Ph.D. and the ARMA Laboratory in Mechanical Engineering, a cooperative robot is being added to improve accuracy. Emerging molecular, gene, and cell-based therapeutics targeting ocular diseases could prevent and potentially reverse cell degeneration and subsequent vision loss. However, reliable and safe delivery of these therapeutics into targeted ocular layers is an ongoing concern, which may affect advancement of these potentially life-changing new treatments. To increase delivery accuracy, reliability, safety and ease of the new molecular therapeutic procedures, we propose to develop B-scan OCT-guided robotic-assisted subretinal therapeutic delivery techniques. The aim is to improve delivery of subretinal injections. Resources through the Vanderbilt Institute for Surgery and Engineering (VISE), the Vanderbilt Vision Research Center (VVRC), the Vanderbilt Biophotonics Center (VBC), and the Vanderbilt Cell Imaging Shared Resource (CISR) permit this collaborative work to occur.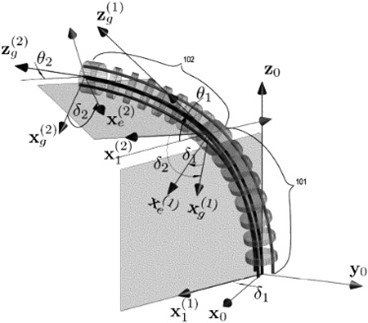
Part of the current robotic OCT surgical research team
Recent Publications:
Simaan N, Del Guidice G, Wang L, Joos K, Shen JH. Continuum Robots with Multi-scale Motion through Equilibrium Modulation. U.S. Patent No. 11,897,129 B2 issued February 13, 2024.
Ahronovich E, Shen JH, Vadakkan TJ, Prasad R, Joos, KM, Simaan N. A five degrees-of-freedom mechanical arm with remote center of motion (RCM) device for volumetric optical coherence tomography (OCT) retinal imaging. Biomedical Optics Express. 15(2):1150-1162, 2024. https://doi.org/10.1364/BOE.505294.
Ahronovich EZ, Simaan N, Joos KM. A review of robotic and OCT-aided systems for vitreoretinal surgery. Adv Ther. 2021 Apr 3. doi: 10.1007/s12325-021-01692-z. Online ahead of print. PMID: 33813718
Del Giudice G, Orekhov AL, Shen J, Joos KM, Simaan N. Investigation of Micro-motion Kinematics of Continuum Robots for Volumetric OCT and OCT-guided Visual Servoing. IEEE/ASME Transactions on Mechatronics, 2021 Oct;26(5):2604-2615. doi: 10.1109/tmech.2020.3043438. PMID: 34658616 PMCID: PMC8519402
Del Giudice, G, Shen JH, Joos K, Simaan N. Feasibility of Volumetric OCT Imaging using Continuum Robots with Equilibrium Modulation, In Deligianni F, Dagnino G, Yang GZ (Eds.), Proceedings of the 12th Hamlyn Symposium on Medical Robotics, June 2019.
Joos K and Shen JH. Optical Coherence Tomography Probe. U.S. Patent No. 9,757,038 issued September 12, 2017.
Del Giudice G, Wang L, Shen JH, Joos K, Simaan N. Continuum Robots for Multi-Scale Motion: Micro-Scale Motion through Equilibrium Modulation. Proceedings of the 2017 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS 2017). Sept 2017, doi: 10.1109/IROS.2017.8206074.
Malone JD, El-Haddad MT, Bozic I, Tye LA, Majeau L, Godbout N, Rollins AM, Boudoux C, Joos KM, Patel SN, Tao YK. Simultaneous multimodal ophthalmic imaging using swept-source spectrally encoded scanning laser ophthalmoscopy and optical coherence tomography. Biomed Opt Express. 2017;8(1):193-206. doi: 10.1364/BOE.8.000193. PMID: 28101411
Yu H, Shen JH, Joos KM, Simaan N. Calibration and integration of B-mode optical coherence tomography for assistive control in robotic micro-surgery. Transactions in Mechatronics. 2016 June 22. [Epub ahead of print], 2016; 21(6):2613-2623. doi: 10.1109/TMECH.2016.2583259. http://ieeexplore.ieee.org/document/7496970/.
.
II. The second program is designed to investigate the role of molecular pathways and genetics in glaucoma. Collaborations are with Human Genetics and the Undiagnosed Disease Network. Part I: The Vanderbilt BioVU and Global Biobank Meta-analysis Initiative (GBMI) resources permitted the discovery of novel glaucoma-associated and ancestry-related gene variants. Recruitment of additional Biobanks is ongoing for additional analyses including incorporating de-identified health EHR information. Part II: Approaches include intraocular pressure measurements, next-generation sequencing, immunohistochemistry, Western blots, and real-time PCR in a laboratory model to evaluate select gene products are ongoing. Part III: Pediatric glaucoma research. Genetics of puzzling pediatric glaucoma cases have been and currently are being examined through the Undiagnosed Diseases Network (UDN).
Part of the international research team that has identified ancestry- and sex-specific genetic loci associated with glaucoma. (photo by Donn Jones)
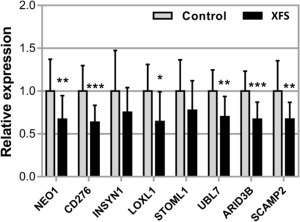
Expression of NEO1, CD276, INSYN1, LOXL1, STOML1, UBL7, ARID3B and SCAMP2 mRNA in iris tissues derived from normal human donors (control) (n = 19) and donors with XFS syndrome (n = 12) using real-time PCR technology. Expression levels were reduced in XFS specimens compared to control specimens, with significant differences for NEO1, CD276, LOXL1, UBL7, ARID3B and SCAMP2. The relative expression levels were normalized relative to GAPDH and are represented as mean values ± SD (*p < 0.05; **p < 0.01, ***p < 0.001)
From https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-023-09179-7
Recent Publications
Lo Faro V, Bhattacharya A, Zhou W, Zhou D, Wang Y, Läll K, Kanai M, Lopera-Maya E, Straub P, Pawar P, Tao R, Zhong X, Namba S; Global Biobank Meta-analysis Initiative; Sanna S, Nolte IM, Okada Y, Ingold N, MacGregor S, Snieder H, Surakka I, Shortt J, Gignoux C, Rafaels N, Crooks K, Verma A, Verma SS, Guare L, Rader DJ, Willer C, Martin AR, Brantley MA Jr, Gamazon ER, Jansonius NM, Joos K, Cox NJ, Hirbo J. Novel ancestry-specific primary open-angle glaucoma loci and shared biology with vascular mechanisms and cell proliferation. Cell Reports Medicine. 5(2):101430. 2024. doi: 10.1016/j.xcrm.2024.101430. PMID: 38382466.
Furuta Y, Tinker RJ, Gulsevin A, Neumann SM, Hamid R, Cogan JD, Rives L, Joos KM, Phillips JA, III, and the Undiagnosed Diseases Network, Probable digenic inheritance of Diamond-Blackfan Anemia. Am J Med Genet A. 194(3):e63454. pp. 1-6, 2024. doi: 10.1002/ajmg.a.63454. Epub 2023 Oct 27. PMID: 37897121.
Fossum K, Knight TJ, Morrison DG, Joos KM. Lensectomy as Treatment for Refractory or Progressive Retinopathy of Prematurity Narrow-Angle Glaucoma. Journal of Pediatric Ophthalmology and Strabismus. 2024 Feb 25:103854. doi: 10.1016/j.jaapos.2024.103854. Online ahead of print. PMID: 38412916.
Elkholey K, Whaba A, Saleem M, Kirabo A, Joos KM, Shibao CA, Biaggioni I. Clinical-Pathological Conference - Post-COVID-19 Baroreflex Failure. Hypertension, 2023, Feb 20. Volume 80, Issue 5, May 2023; Pages 895-900, https://doi.org/10.1161/HYPERTENSIONAHA.123.20316 PMID: 36802914.
Hirbo JB, Pasutto F, Gamazon ER, Evans P, Pawar P, Berner D, Sealock J, Tao R, Straub PS, Anuar I. Konkashbaev AI, Breyer M, Schlötzer-Schrehardt U, Reis A, Brantley Jr MA., Khor CC, Joos KM, Cox NJ. Analysis of genetically determined gene expression suggests role of inflammatory processes in exfoliation syndrome. BMC Genomics, 2023 Feb 16;24(1):75. doi: 10.1186/s12864-023-09179-7. PMID: 36797672.
Shibao C, Joos K, Phillips JA 3rd, Cogan J, Newman JH, Hamid R, Meiler J, Capra J, Sheehan J, Vetrini F, Yang Y, Black B, Diedrich A, Roberston D, Biaggioni I. Familial Autonomic Ganglionopathy Caused by Rare CHRNA3 Genetic Variants. Neurology. 2021 May 4:10.1212/WNL.0000000000012143. doi: 10.1212/WNL.0000000000012143. Online ahead of print. PMID: 33947782.
Papadopoulos M, Vanner EA, Grajewski A, and ISOCG CGRN Study Group [Arijit Mithra, Manju Pillai, Swati Upadhyaya, Ganesh Venkataraman (Aravind Eye Hospital, India); Ta Chen Peter Chang, Alana Grajewski, Elizabeth Hodapp (Bascom Palmer Eye Institute, USA); Velota Sung (Birmingham and Midland Eye Centre, UK commenced 6/8/13); Orna Geyer, Alvit Wolf (Carmel Medical Center, Israel commenced 6/3/14); Ellen Mitchell, Ken Nischal (Children's Hospital of Pittsburgh, USA); Sharon Freedman (Duke Eye Center, USA); Allen Beck, Annette Giangiacomo (Emory Eye Center, USA), Anne Coleman (Jules Stein Eye Institute, USA); Arif Khan (King Khaled Eye Specialist Hospital, Saudi Arabia); Anil Mandal, Sirisha Senthil (LV Prasad Eye Institute, India); John Brookes, Peng Tee Khaw, Maria Papadopoulos (Moorfields Eye Hospital, UK); Jocelyn Chua, Ching Lin Ho (Singapore National Eye Center, Singapore); James Brandt (UC Davis Eye Center, USA); Vera Essuman (Korle-Bu Teaching Hospital, Ghana commenced 12/12/13); Ray Areaux, Elena Bitrian, Alana Grajewski (University of Minnesota, USA); Franz Grehn, Thomas Klink (University Hospital Würzburg, Germany); Karen Joos (Vanderbilt Eye Institute, USA)]. International Study of Childhood Glaucoma (ISOCG), Ophthalmology Glaucoma. 2020;3(2):145-157. epub jan 2, 2020 DOI: https://doi.org/10.1016/j.ogla.2019.12.007.
Morgan TM, Colazo JM, Duncan L, Hamid R, Joos KM. Two cases of oculofaciocardiodental (OFCD) syndrome due to X-linked BCOR mutations presenting with infantile hemangiomas: phenotypic overlap with PHACE syndrome, Case Reports in Genetics. 2019 Dec 28;2019:9382640. doi: 10.1155/2019/9382640. eCollection 2019. PMID: 31956451.
Grossman AL, Javitt MJ, Moster SJ, Grajewski AL , Pediatric Glaucoma Subcommittee of the American Glaucoma Society (Beck AD, Blieden LS, Bitrian E, Chang TC, Freedman SF, Hodapp E, Joos KM, Reiser BJ, Tanna AP) American Glaucoma Society position statement on cannabinoid use in pediatric glaucoma patients. Ophthalmology Glaucoma. 2019;2:365-366.
Tan B, Gurdita A, Choh V, Joos K, Prasad R, Bizheva K. Morphological and functional changes in the rat retina associated with 2 months of intermittent moderate intraocular pressure elevation. Scientific Reports. 2018; 8:7727 (1-11) . doi:10.1038/s41598-018-25938-zwww.nature.com/articles/s41598-018-25938-z, PMID: 29769654.
Choh V, Gurdita A, Tan B, Feng Y, Bizheva K, McCulloch DL, Joos KM. Isoflurane and ketamine:xylazine differentially affect intraocular pressure-associated scotopic threshold responses in Sprague-Dawley rats. Doc Ophthalmol. 2017;135(2):121-132. doi: 10.1007/s10633-017-9597-7. PMID: 28638951.
Gurdita A, Tan B, Joos KM, Bizheva K, Choh V. Pigmented and albino rats differ in their responses to moderate, acute and reversible intraocular pressure elevation. Doc Ophthalmol. 2017 Apr 7. doi: 10.1007/s10633-017-9586-x. [Epub ahead of print] PMID: 28389912.
Nathan N, Joos KM. Glaucoma disparities in the Hispanic population. Seminars in Ophthalmology 2016 Apr 29:1-6. [Epub ahead of print] PMID: 27128326.
Choh V, Gurdita A, Tan B, Prasad RC, Bizheva K, Joos KM. Short-term moderately elevated intraocular pressure is associated with elevated scotopic electroretinogram responses. Investigative Ophthalmology and Visual Science, 2016; 57(4): 2140-2151. doi: 10.1167/iovs.15-18770. PMID: 27100161.