Biopsychosocial Impacts on Urinary Function and Behavior
This research area examines how psychology and urinary symptoms and conditions interact and forms the basis for an emerging, multidisciplinary field combining urology and psychology, i.e. “uropsychology.”
Dr. Reynolds’ R01 (R01DK129624 Stress and Anxiety Effects on Overactive Bladder: A Controlled Study) was recently funded by NIH/NIDDK. This R01 studies the impacts of psychological stress and anxiety on acute bladder sensitivity, urinary symptoms, and compensatory bladder behaviors in men and women with OAB in a controlled laboratory setting and everyday situations. The project uses cutting edge methods for measuring bladder sensations and responses to acute, invoked laboratory psychological stress as well as state-of-the-art techniques in Ecological Momentary Assessment (EMA).
Interested in participating or learning more? Click here to see if you qualify.
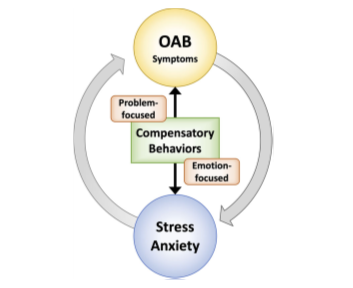
FIGURE 3 Conceptual model. OAB symptoms and emotional states (i.e., stress and anxiety) interact in a feed‐forward, cyclical relationship (gray arrows). Compensatory behaviors can modulate this relationship (black arrows) by decreasing OAB symptoms (i.e., problem‐focused coping behaviors) or by alleviating emotional responses (i.e., emotion‐focused coping behaviors). Reduced emotional distress then reinforces the compensatory behaviors, making them more likely to occur again in the future. From Reynolds et al, Neurourology and Urodynamics, 2021.
Selected Publications
Reynolds WS, McKernan LC, Dmochowski RR, Bruehl S. The biopsychosocial impacts of anxiety on overactive bladder in women. Neurourol Urodyn. 2023 Feb 13. doi: 10.1002/nau.25152. PMID: 36780135
Reynolds WS, Fowke J, Dmochowski RR. The Burden of Overactive Bladder on US Public Health. Current Bladder Dysfunction Reports. 2016, 11 (1): 8-13. PMID: 27057265. PMCID: PMC4821440.
McKernan LC, Walsh CG, Reynolds WS, Crofford LJ, Dmochowski RR, Williams DA. (2018). Psychosocial co-morbidities in Interstitial Cystitis/Bladder Pain syndrome (IC/BPS): A systematic review Neurourology Urodynamics. 37(3): 926–941. PMID: 28990698. PMCID: PMC6040587.
McKernan LC, Johnson BN, Reynolds WS, Williams DA, Cheavens JS, Dmochowski RR, Crofford LJ (2019). Posttraumatic Stress Disorder in Interstitial Cystitis/Bladder Pain Syndrome: Relationship to Patient Phenotype and Clinical Practice Recommendations. Neurourology and Urodynamics; 38(1):353-362. PMID: 30350890. PMCID: PMC6310618
McKernan LC, Crofford LJ, Kim A, Vandekar SN, Reynolds WS, Hansen KA, Clauw DJ, Williams DA (2021). Electronic Delivery of Pain Education for Chronic Overlapping Pain Conditions: A Prospective Cohort Study. Pain Med. [Epub 2021 Jan 27]. PMID: 33871025.
Reynolds WS, Kaufman MR, Bruehl S, Dmochowski RR, McKernan LC (2021). Compensatory Bladder Behaviors (“Coping”) in Women with Overactive Bladder. Neurourology and Urodynamics. [Epub September 15, 2021]. PMID: 34524704. PMCID: in process.


