Interstitial cystitis and bladder pain
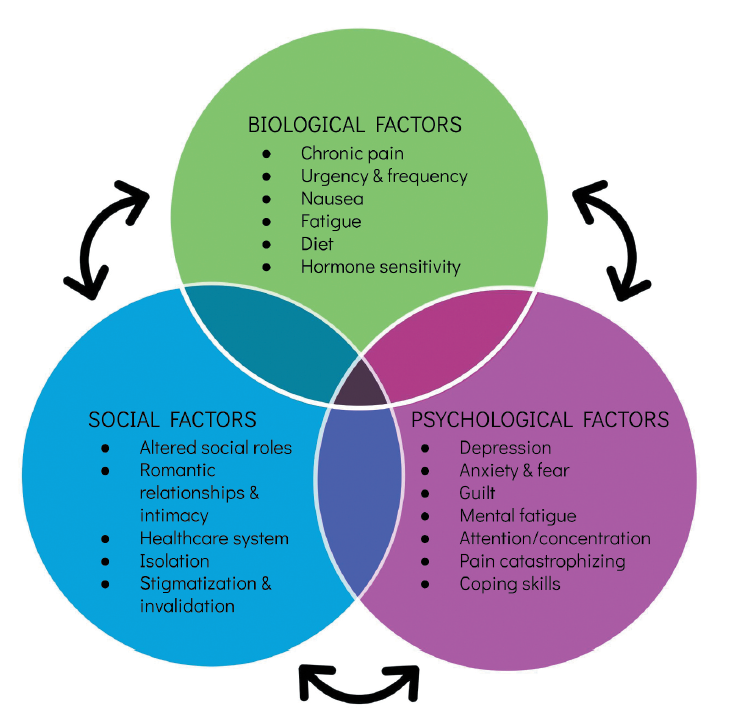
Through clinical experience, the urology team has found that using a multidisciplinary approach to treat interstitial cystitis/bladder pain syndrome best meets our patient needs. Everyone has a unique symptom presentation. During visits in the IC/BPS clinic, we work to explore your symptoms, triggers, history, and also the different ways in which IC/BPS is impacting your life. This includes an assessment of your physical and emotional wellness. In doing so, we are able to construct a treatment plan that best meets your needs. Initial visits are conducted together with an experienced nurse practitioner who has worked with IC for decades, a health psychologist who specializes in IC/BPS and chronic pain, and a surgeon available for procedural consultations as needed. VUMC also has a team of pelvic floor physical therapists who often work closely with us in implementing treatment plans. We find that having health psychology present can help to provide additional services to help facilitate in-office procedures, which patients report benefitting from.
This work is also the topic of Dr. McKernan’s research, which you can find more information regarding here.
Relevant Publications
- McKernan, L.C., Bonnett, K., Finn, M.T.M., Schlundt, D., Williams, D.A., Bruehl, S., Clauw, D., Dmochowski, R.R., Reynolds, W.S., & Crofford, L.J. Qualitative Analysis of Treatment Needs in Interstitial Cystitis/Bladder Pain Syndrome: Implications for Intervention. Canadian Journal of Pain. (attached, full text here: https://www.tandfonline.com/doi/full/10.1080/24740527.2020.1785854 )
- Windgassen, S. & McKernan, L.C. Cognition, Emotion, and the Bladder: Psychosocial Factors in Bladder Pain Syndrome and Interstitial Cystitis (2020). Current Bladder Dysfunction Reports, 15, 9-14. DOI: 10.1007/s11884-019-00571-2 full text here: https://link.springer.com/article/10.1007/s11884-019-00571-2
- McKernan, L.C., Johnson, B.N., Crofford, L., Lumley, M.A., Bruehl, S., & Cheavens, J.C. (2019) Posttraumatic Stress Symptoms Mediate the Effects of Trauma Exposure on Clinical Indicators of Central Sensitization in Patients with Chronic Pain. Clinical Journal of Pain, 35(5), 385-393. DOI:10.1097/AJP.0000000000000689. full text here: https://www.researchgate.net/profile/Benjamin_Johnson5/publication/331118513_Posttraumatic_Stress_Symptoms_Mediate_the_Effects_of_Trauma_Exposure_on_Clinical_Indicators_of_Central_Sensitization_in_Patients_With_Chronic_Pain/links/5e8f9be64585150839ceac5f/Posttraumatic-Stress-Symptoms-Mediate-the-Effects-of-Trauma-Exposure-on-Clinical-Indicators-of-Central-Sensitization-in-Patients-With-Chronic-Pain.pdf
- McKernan, L.C., Johnson, B.N., Reynolds, W.S., Williams, D.A., Cheavens, J.S., Dmochowski, R.R., & Crofford, L.J. (2018). Posttraumatic Stress Disorder in Interstitial Cystitis/Bladder Pain Syndrome: Relationship to Patient Phenotype and Clinical Practice Implications. Neurourology and Urodynamics. DOI: 10.1002/nau.23861. PMID: 30350890 full text here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6310618/
- McKernan, L.C., Walsh, C.G., Reynolds, W.S., Dmochowski, R.R., Crofford, L., & Williams, D.A. (2017). Psychosocial Co-Morbidities in Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS): A Systematic Review. Neurourology and Urodynamics, 1-16, DOI: 10.1002/nau.23421. full text here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6040587/