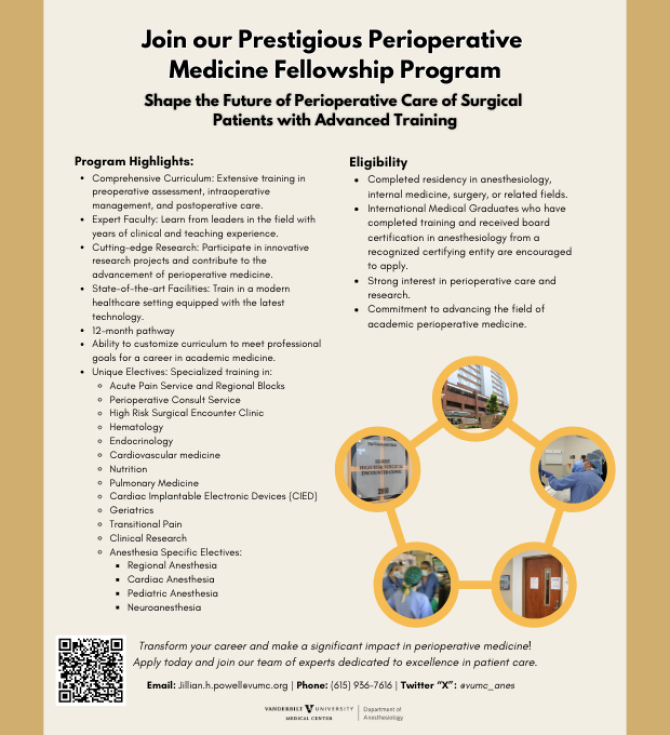
The Department of Anesthesiology is excited to announce a new Fellowship in Perioperative Medicine. The term perioperative medicine describes the non-surgical care of patients from the time surgery is considered through the perioperative period and to full recovery. In the practice of perioperative medicine, many medical specialties work in concert to provide optimal outcomes for surgical patients. The medical knowledge distinct to this field includes that of surgical and anesthesia risks and complications, patient-specific risks due to co-morbid medical conditions, and methods by which to reduce risk and manage medical illness in the perioperative period.
The evidence supporting the value of best practices in perioperative medicine is rapidly expanding, and the full spectrum of this domain of medicine is not covered in any core residency program. In light of this, the Department of Anesthesiology’s innovative new fellowship program is designed to place trainees at the forefront of this important area of medicine, preparing them to provide personalized precision perioperative care. As one example, if postoperative mortality from cardiac causes (within 30 days of surgery) was considered as a disease entity, it would be the third leading cause of death among adults in the United States. Knowledge of how to properly assess risk and manage medical comorbidities throughout the entire perioperative period stands to make significant improvement in the highest risk patients.
The Perioperative Medicine Fellowship was created with input from a multi-disciplinary team at Vanderbilt, including faculty from the Departments of Anesthesiology, Medicine, and Surgery. It is a one-year program that will train participants to be leaders in the clinical and academic research components of their professions, teaching them the skills needed to implement and manage their own perioperative consult service upon completion. Up to four trainees will be admitted into the fellowship each year. During the fellowship program, participants can expect to gain experience in the following core rotations: Perioperative Consult Service, High-Risk Preoperative Evaluation Clinic, Echocardiography and Cardiac Implantable Electronic Device Management, Research, and a wide variety of electives.
One unique aspect of this new fellowship offering is that it is open to those who have completed an ACGME-accredited residency program in anesthesiology or in general surgery. Furthermore, faculty instructors in the program come from the VUMC Departments of Anesthesiology, Surgery, and Medicine, making this a truly cross-departmental educational effort - mirroring the collaboration inherent to the concept of perioperative medicine.
Applications are now being accepted for training to start in August 2020. To learn more about the new Perioperative Medicine Fellowship, including information on how to apply, visit the Department of Anesthesiology’s website at www.vandydreamteam.com.
-
We are now accepting applications for the academic years beginning July 2020 and July 2021.
To be considered, all potential fellows must have completed an ACGME-accredited residency program in Anesthesiology or General Surgery OR be a current Anesthesiology or General Surgery resident in good standing and targeted for residency completion prior to the fellowship start date.
Application Requirements
To apply, please provide the following to Jillian Powell at jillian.h.powell@vumc.org :- Completed application.
- Cover letter with personal statement and preferred start date.
- Transcript from medical school.
- Official licensure verification from all states in which you have been or are currently licensed.
- USMLE and ITE scores.
- Three (3) letters of recommendation, one of which must be from your current program director or equivalent (i.e., Division Chief or Department Chair for those applicants currently in practice).
- Click here to view flyer.

- Click here to view the flyer with program details.
-
2021
An improved predictive model for postoperative pulomonary complications after free flap reconstructions in the head and neck
Smith, DK, Freundlich RE, Shinn JR, Wood CB, Rohde SL, McEvoy MD.
Head Neck. 2021 Mar 30. doi: 10.1002/hed.26689. Online ahead of print.
PMID: 33783905The Electrophysiology Laboratory: Anesthetic Considerations and Staffing Models.
Siegrist KK, Fernandez Robles C, Kertai MD, Oprea AD.
J Cardiothorac Vasc Anesth. 2021 Feb 26:S1053-0770(21)00185-3. doi: 10.1053/j.jvca.2021.02.050. Online ahead of print.
PMID: 33773891 Review.Motoric Subtypes of Delirium and Long-Term Functional and Mental Health Outcomes in Adults After Critical Illness.
Rengel KF, Hayhurst CJ, Jackson JC, Boncyk CS, Patel MB, Brummel NE, Shi Y, Shotwell MS, Ely EW, Pandharipande PP, Hughes CG.
Crit Care Med. 2021 Feb 23. doi: 10.1097/CCM.0000000000004920. Online ahead of print.
PMID: 33729717Unanticipated Consequences of Switching to Sugammadex: Anesthesia Provider Survey on the Hormone Contraceptive Drug Interaction.
Dwan RL, Raymond BL, Richardson MG.
Anesth Analg. 2021 Mar 8. doi: 10.1213/ANE.0000000000005465. Online ahead of print.
PMID: 33684087Potential Renoprotective Strategies in Adult Cardiac Surgery: A Survey of Society of Cardiovascular Anesthesiologists Members to Explore the Rationale and Beliefs Driving Current Clinical Decision-Making.
McIlroy DR, Roman B, Billings FT 4th, Bollen BA, Fox A, Geube M, Liu H, Shore-Lesserson L, Zarbock A, Shaw AD.
J Cardiothorac Vasc Anesth. 2021 Feb 6:S1053-0770(21)00099-9. doi: 10.1053/j.jvca.2021.02.004. Online ahead of print.
PMID: 33674203Predictive Accuracy of a Polygenic Risk Score for Postoperative Atrial Fibrillation After Cardiac Surgery.
Kertai MD, Mosley JD, He J, Ramakrishnan A, Abdelmalak M, Hong Y, Shoemaker MB, Roden DM, Bastarache L.
Circ Genom Precis Med. 2021 Mar 1. doi: 10.1161/CIRCGEN.120.003269. Online ahead of print.
PMID: 336472232020
Screening Asymptomatic Kidney Transplant Candidates-Primum Non Nocere.
Beckman JA, McEvoy MD.
JAMA Intern Med. 2020 Oct 1;180(10):1366-1367. doi: 10.1001/jamainternmed.2020.2674.
PMID: 32777003 No abstract available.Association of neuronal repair biomarkers with delirium among survivors of critical illness.
Hayhurst CJ, Patel MB, McNeil JB, Girard TD, Brummel NE, Thompson JL, Chandrasekhar R, Ware LB, Pandharipande PP, Ely EW, Hughes CG.
J Crit Care. 2020 Apr;56:94-99. doi: 10.1016/j.jcrc.2019.12.010. Epub 2019 Dec 16.
PMID: 31896448 Free PMC article.2018
Evidence Review Conducted for the Agency for Healthcare Research and Quality Safety Program for Impriving Surgical Care and Recovery: Focus on Anesthesiology for Bariatric Surgery
Use of American College of Surgeons National Surgical Quality Improvement Program Surgical Risk Calculator During Preoperative Risk Discussion: The Patient PerspectiveAn enhanced recovery program in colorectal surgery is associated with decreased organ level rates of complication: a difference-in-differences analysis
An enhanced recovery program for bariatric surgical patients significantly reduces perioperative opioid consumption and postoperative nausea.
Enhanced Recovery Pathway in Microvascular Autologous Tissue-Based Breast Reconstruction: Should It Become the Standard of Care?
Competence: The Link between Education and Quality Patient Care.
American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Nutrition Screening and Therapy Within a Surgical Enhanced Recovery Pathway.
American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Postoperative Gastrointestinal Dysfunction Within an Enhanced Recovery Pathway for Elective Colorectal Surgery.
American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Patient-Reported Outcomes in an Enhanced Recovery Pathway.
Cardiac Arrest in the Operating Room: Resuscitation and Management for the Anesthesiologist: Part 1.
Cardiac Arrest in the Operating Room: Part 2-Special Situations in the Perioperative Period.
2017
Mobile Technology in the Perioperative Arena: Rapid Evolution and Future Disruption.
A Quick Look Into the Future: Focused Cardiovascular Ultrasound (FCU).
Anesthesiologists: Physicians to the System.
Perioperative Medication Management.
2016
Surgical Apgar score is associated with myocardial injury after noncardiac surgery.
Education in Anesthesiology: Is It Time to Expand the Focus?
Disruptive Education: Training the Future Generation of Perioperative Physicians.
Postoperative Ketamine: Time for a Paradigm Shift.
Education in Anesthesiology: Is It Time to Expand the Focus?
Perioperative and Acute Care Transfusion Strategies: One size may not fit all.
Observational Research Using Propensity Scores.
2015
Why Have So Many Intravascular Glucose Monitoring Devices Failed? Dialogue on the Future of Anesthesiology. The Future of Anesthesiology: Should the Perioperative Surgical Home Redefine Us? A Brief History of the Perioperative Surgical Home. Perioperative transfusion: a complicated story.
-
Anesthesiology Team Members

Brian Allen, MD
Perioperative Consult Service

Holly Ende, MD
Hi-RiSE Clinic Team
Kevin Furman, DO
Perioperative Consult Service
Alexander George, MD
Perioperative Consult Service
Christina Hayhurst, MD
Perioperative Consult Service

Miklos Kertai, MD, PhD
Hi-RiSE Clinic Team

Merrick Miles, MD
Perioperative Consult Service

Dorothee Mueller, MD
Perioperative Consult Service

Kimberly Rengel, MD
Hi-RiSE Clinic Team
Amy Robertson, MD
Hi-RiSE Clinic Team
Jeremy Walco, MD
Hi-RiSE Clinic Team

Sheena Weaver, MD
Perioperative Consult Service
Hi-RiSE Clinic TeamMedical and Surgical Team Members

Josh Beckman, MD, MS
Cardiology

Chris Biesemeier
Nutrition

Rosemarie Dudenhofer, MD
Pulmonary/Sleep Medicine

Mariu Duggan, MD
Geriatrics

Maie El-Sourady, MD
Hospice
Palliative Medicine

Michael Fowler, MD
Endocrinology

Tim Geiger, MD, MMHC
Colorectal Surgery

Kamran Idrees, MD, MSCI
Surgical Oncology

Lisa Lillie, MS-MPH, RD, LDN
Nutrition

David Marcovitz, MD
Addiction Psychiatry

Colleen Morton, MBBCh
Hematology

Carla Sevin, MD
Pulmonary Medicine

Myrick Shinall, MD, PhD
Surgical Pallative Care
Hillary Tindle, MD, MPH
Smoking Cessation