How good is your memory? Debating the duration of COVID-19 immunity.
In today’s COVID-19-centric world, it is easy to feel overwhelmed by headlines constantly broadcasting differing timelines of just how long this pandemic could last. One main determinant of the duration of lockdowns and social distancing is the development of a vaccine. As described in Chris Hofmann’s article on vaccine development, the goal is “to create a vaccine that is safe and with good immunogenicity, meaning it stimulates a strong immune response.” Recent developments of COVID-19 vaccine design have promised ≥90% effectiveness, however, we are still missing the second half of the story. It is one achievement to instill COVID-19 immunity in the majority of vaccine recipients, but another to maintain this protection. Concernedly, news outlets including top tier science journals such as Nature and Science have been reporting conflicting numbers on just how long we can expect COVID-19 immunity to last, in other words, how long an individual can go before being re-infected with the virus. It is important to note that a majority of these study reports have yet to be put through peer review due to the rapidly developing nature of the pandemic, however, we can still compile study results to predict the duration of COVID-19 immunity.
Discrepancies in the lifetime of COVID-19 antibodies
At the end of October, one study from the United Kingdom, which followed upwards of 350,000 individuals, reported that conferred immunity appeared to be weak and short-lasting, with 25% of study participants losing immunity only 3 months into the study1. The release of this research report fueled multiple large and influential news outlets to proclaim that COVID-19 immunity falls alarmingly fast. This article appeared to be supported by an earlier study out of China reporting a sole 1 month of immunity2, however, not weeks later, two separate peer-reviewed reports came out in Science and The New England Journal of Medicine describing that the majority of 30,000 study participants had lasting immunity for 4-5 months3. Yet another article touted immunity lasting up to 6 months at the start of November, and the latest news reports 6 months as the minimum time for detecting antibodies4.
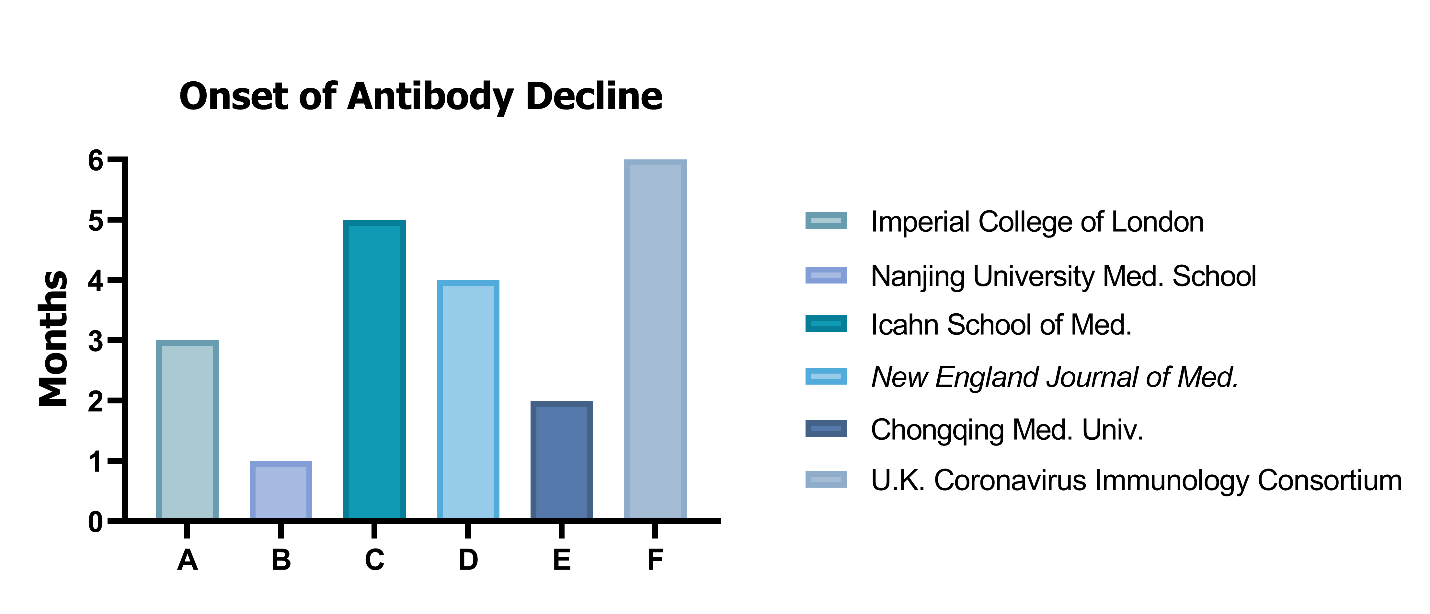
So, what can we believe when it comes to COVID-19 and its lasting immunity? To be sure, we may never have an exact answer to this question, but so far results point to an order of 3-6 months. But this is only half of the story. To truly understand what it means to have “lasting immunity”, we need to take a step back and return to the basis of immunological memory.
Adaptive Immunity: What it is and how it confers resistance to re-infection
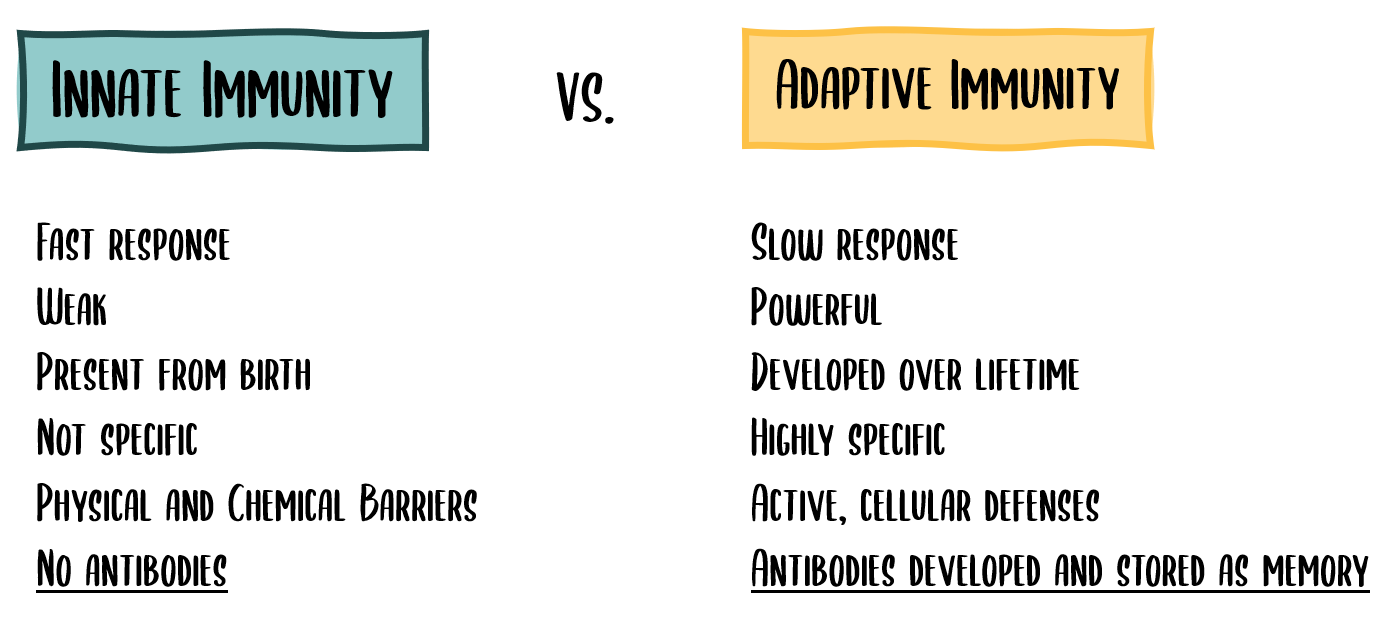
When the immune system first encounters a foreign contaminant, or pathogen, innate immunity takes the initial hit. Innate immunity is a fast response but relies solely on what defenses the body already has in place – mucous membranes in the nose, for example, serve to trap viral particles before they can enter underlying body tissues. Once this innate immunity barrier is breached, however, the body has no choice but to rally antibody-producing cells, known as B cells, and create antibodies specific to the invader. Known as adaptive immunity, this process of building up antibody defenses is slow, yet more powerful. The key to adaptive immunity is that once the invader has been defeated, both B-cells and their antibody stores are depleted save for a small amount that are stored in your blood’s immunological memory supply. In the chance that there is a repeat encounter with the same invader, your immune system can use these memory B cells and stored antibodies from the first attack to create a strong secondary defense much more quickly.
Antibodies, assemble!
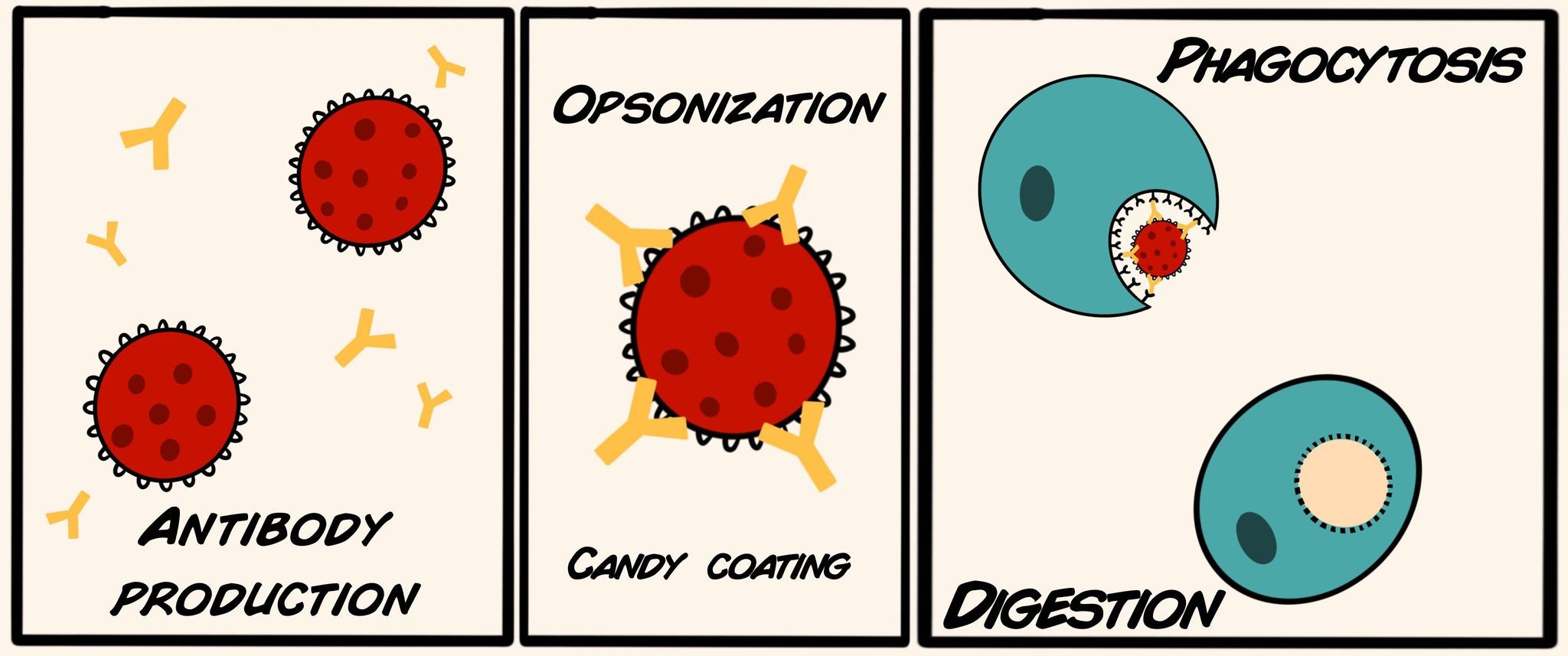
Antibodies are created by immune B cells and are specifically designed to latch onto the invaders’ surfaces. The antibodies function in a process known as opsonization during which they form a “candy coating” around the invader so that it is more recognizable and delectable to a different type of immune cell called a phagocyte. From the Greek word for “eating”, phagocytes engulf invaders marked for destruction by antibodies, and digest them in their acidic environment. Furthermore, when covered by a coat of antibodies, viruses have a hard time attaching to host cell surfaces.
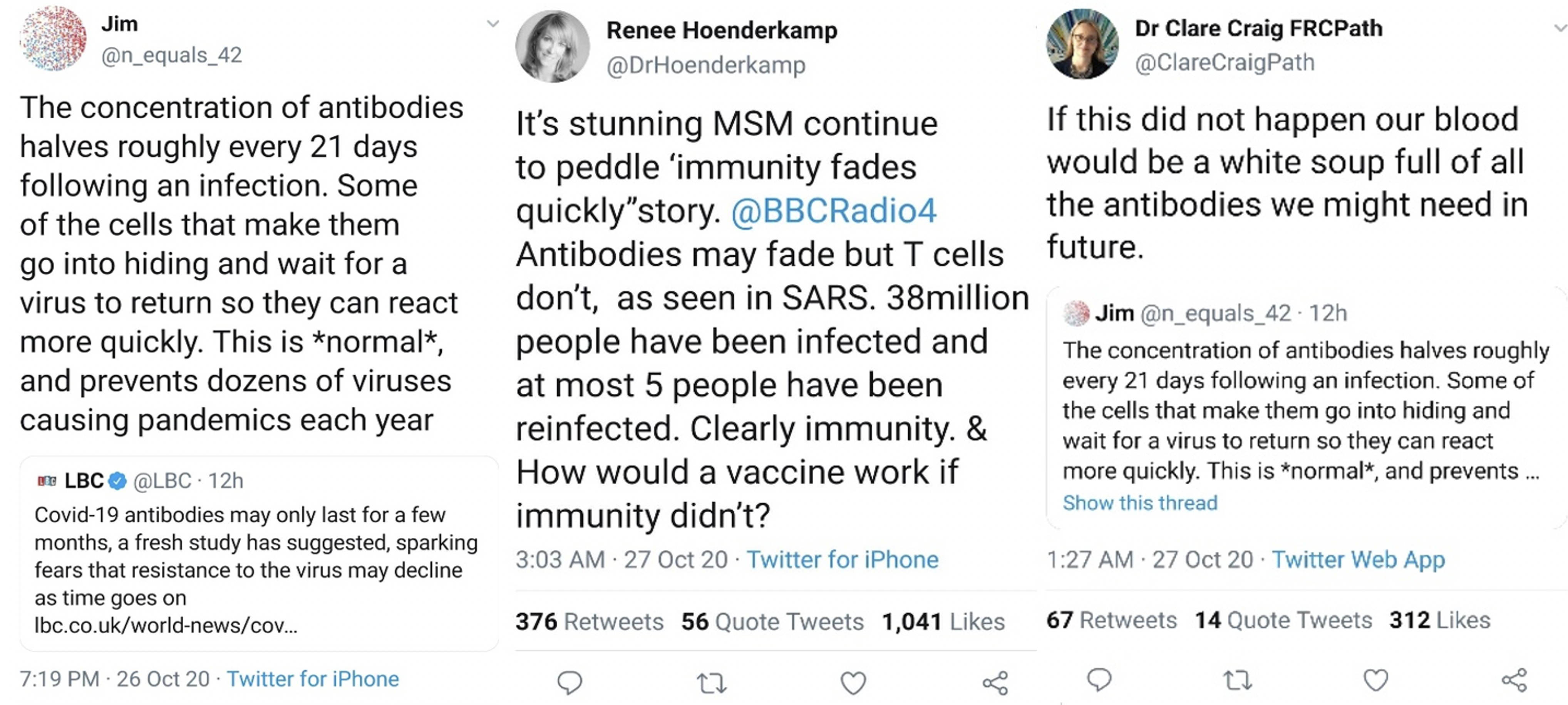
From the Horses’ Mouths: Scientists disagree about fading antibody models
Immunologists on the “Science Side of Twitter” have countered the reports surrounding supposed COVID-19 short-term immunity. Although antibody concentration dwindles within study participants after initial exposure, we know that this is to be expected given the general behavior of the immune system and its memory bank of antibodies. Immunological memory is not a new concept – even the Greek historian, Thucydides, recorded observations that Athenians infected with the plague never were infected twice5. But how many antibody-producing memory B cells can the body store? The storage sites of these cells are known as “secondary lymphoid organs” and include the spleen and lymph nodes. It is estimated that at any given time the body can store up to 15g of antibody per liter of blood depending on the type of antibody6. The combination of lingering antibodies and stored memory B cells allows the immune system to mount its strong secondary response so quickly, that you may not even notice you were ever re-infected.
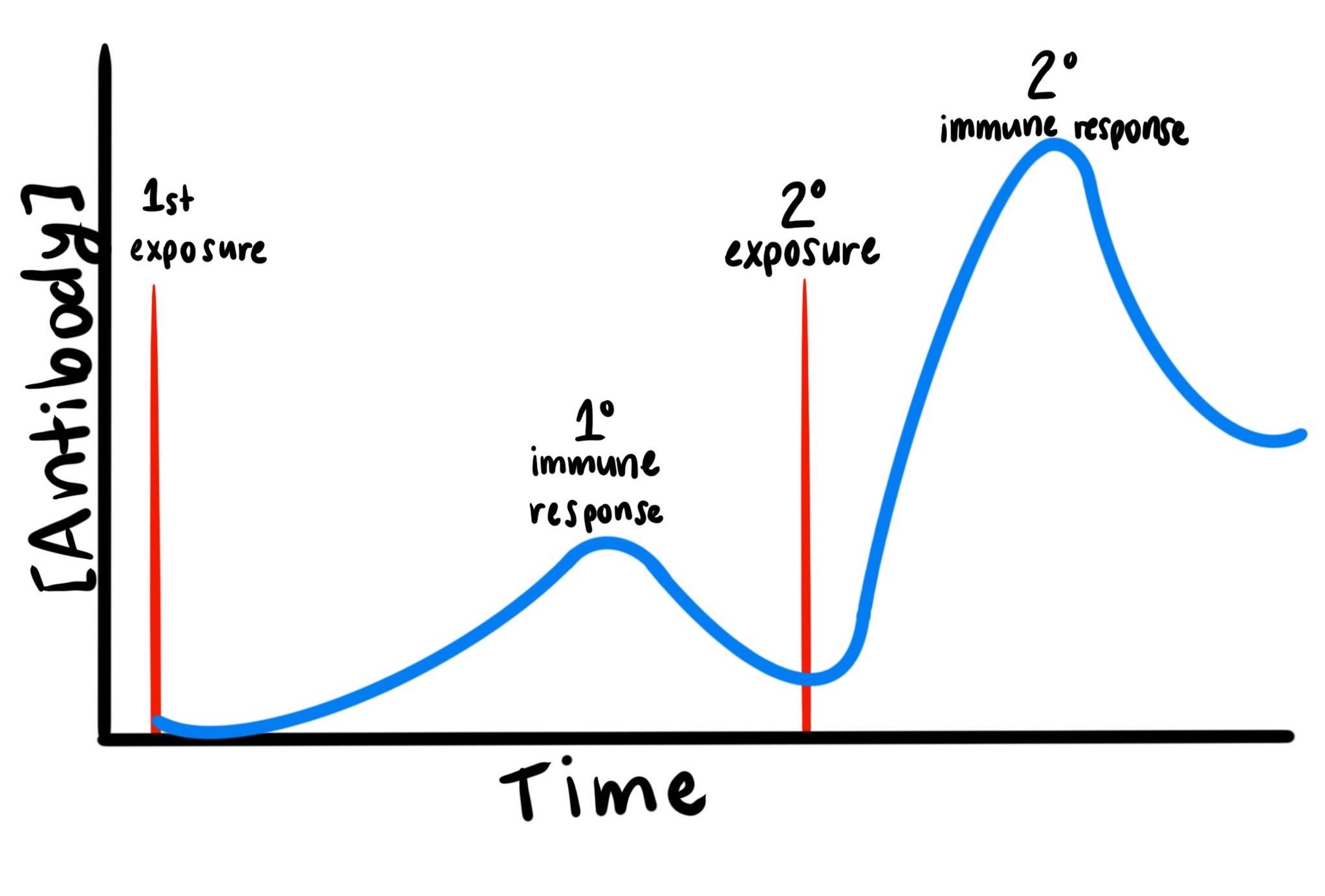
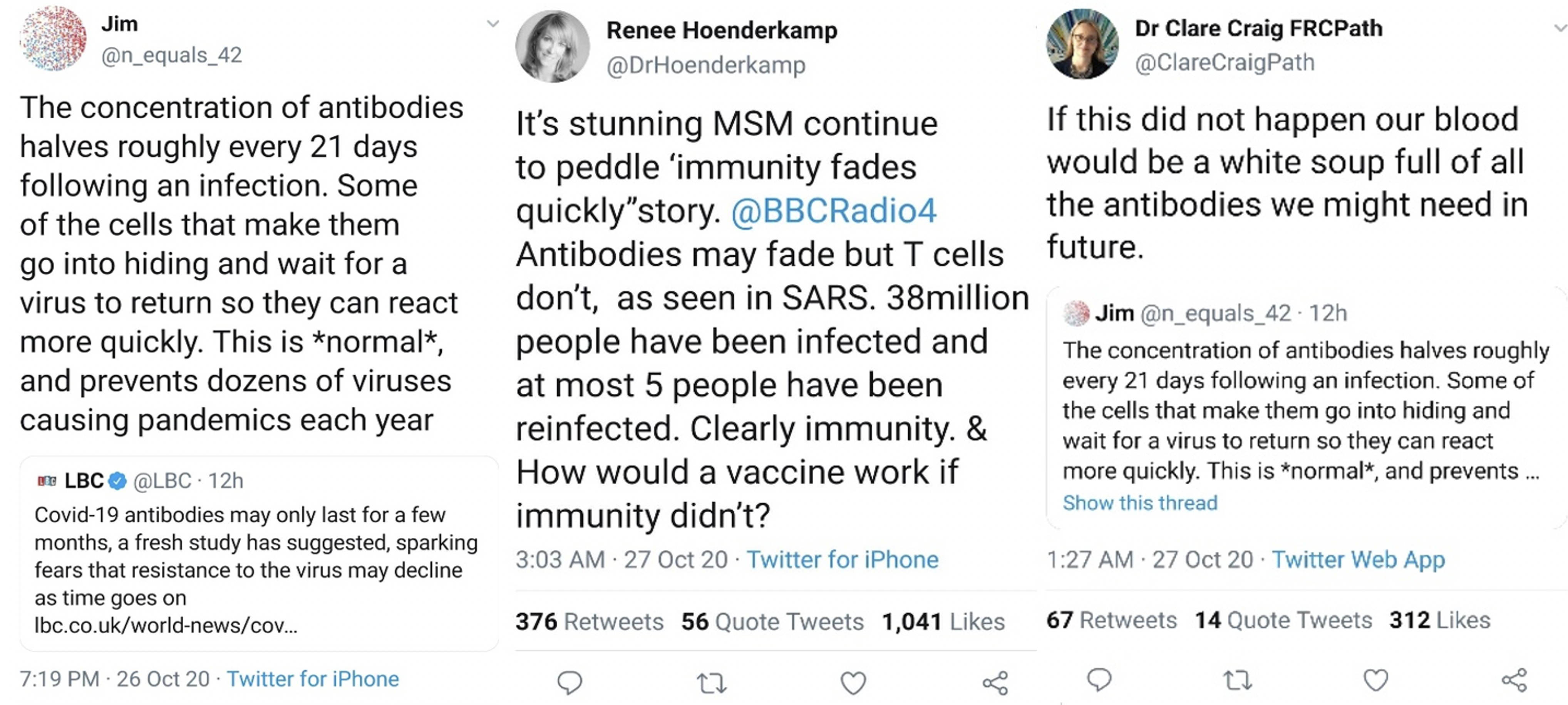
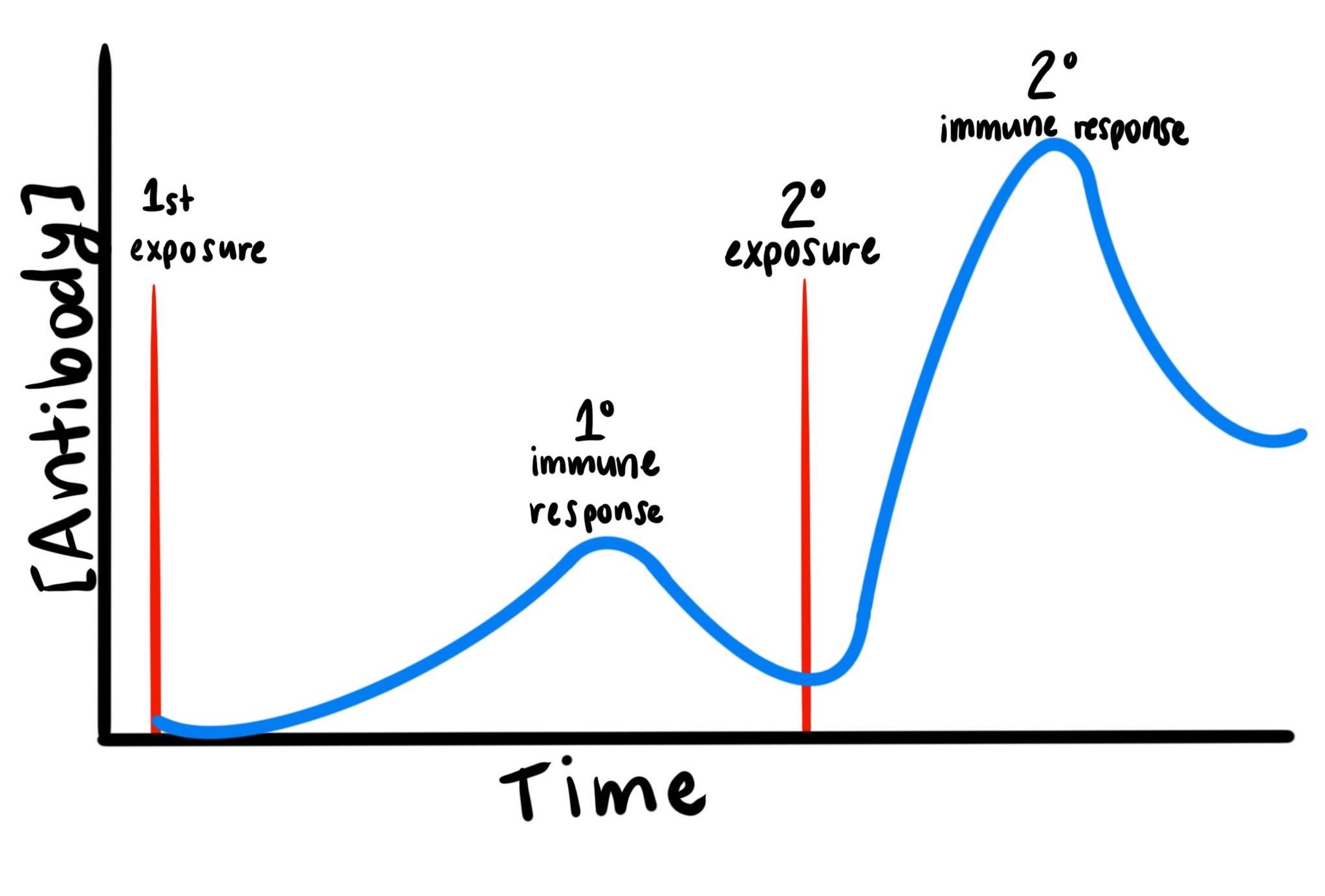
Immunologists on the “Science Side of Twitter” have countered the reports surrounding supposed COVID-19 short-term immunity. Although antibody concentration dwindles within study participants after initial exposure, we know that this is to be expected given the general behavior of the immune system and its memory bank of antibodies. Immunological memory is not a new concept – even the Greek historian, Thucydides, recorded observations that Athenians infected with the plague never were infected twice5. But how many antibody-producing memory B cells can the body store? The storage sites of these cells are known as “secondary lymphoid organs” and include the spleen and lymph nodes. It is estimated that at any given time the body can store up to 15g of antibody per liter of blood depending on the type of antibody6. The combination of lingering antibodies and stored memory B cells allows the immune system to mount its strong secondary response so quickly, that you may not even notice you were ever re-infected.
Natural Herd Immunity is Impossible: Why we need a vaccine
Given prior knowledge about the power of secondary immunity, it will take a vaccine to slow the instance of infection within the population. There have been predictions that herd immunity, naturally acquired from infections alone, could be enough to stop the spread of COVID-19 with no need for a vaccine. However, epidemiological models tell a different story. For example, although New York City experienced a slew of infections during the first wave of the pandemic, scientists state that they are still far from experiencing herd immunity7. There is still over 80% of the city population that is susceptible to the virus. If herd immunity had been reached in New York City, COVID-19 case numbers would be expected to go down, not just hold at a plateaued level8. In order to reach a functioning level of natural herd immunity, it is estimated that at least 70% of the population would have to be recovered – numbers that would risk losing an astounding number of vulnerable lives. Overall, vaccine-mediated herd immunity is the safest and most controlled route that we can take in the fight against COVID-19.
You get a vaccine, you get a vaccine, you get a vaccine! (Or do you?)
With new excitement over the three outstanding vaccines – Pfizer, Moderna, and Oxford – what can we expect to happen next? The outlook is more than good – out of over 40,000 study participants, for example, the Pfizer phase III vaccine trial has recorded only 94 positive COVID-19 cases. The trial directors have not revealed whether these positive cases were within the placebo (control) group or the vaccinated group, but maintain that after 2 doses of the vaccine, it remains over 90% effective9. Pfizer’s vaccine isn’t perfect – it will require a second “booster” shot after 3 weeks to ensure conferred immunity, but it is a strong contender in the fight against COVID-1910.
Not long after news broke over Pfizer’s supposed success in vaccine design, Moderna released their report touting 94.5% efficacy without the need for a booster shot11. Furthermore, Moderna’s design allows for this vaccine to be transported and stored at common refrigeration temperatures as opposed to Pfizer’s, which requires a specialized -80°C freezer – limiting where the Pfizer vaccine could be distributed.
Our third and final candidate, for now, comes from the Oxford-AstraZeneca team. Perhaps the most controversial on the list, this vaccine has had mixed reviews. With phase III reporting 70% efficacy, this pales in comparison to Pfizer and Moderna’s numbers. Additionally, the Oxford vaccine will require a booster shot, with two doses given a month apart. Interestingly, new findings dictate that study participants receiving a partial dose followed by a full dose, for the booster, were 90% less likely to develop COVID-19 than the placebo group12.