SPOTLIGHT: Gregory Harrington, BA, RN4
CCL Holding Room/ EP PACU CCT5
Vanderbilt Medical Center
Type of project: EBP implementation and Research/evaluation of outcomes
Title of project: Atrial Fibrillation Back Pain Study
Description of project:
Due to the nature of the pre, intra, and post procedure processes, a very consistent complaint from our patient population is back pain. Most of our patients spend greater than an hour lying in a stretcher before procedure, another 1-4 hours in procedure, and 2-6 hours post-procedure. Our protocols state that the pt. needs to be flat for the entire time they are in procedure and post procedure.
Why you chose this project:
After speaking with several RNs, patients, and even one RN and one provider that had recently been through an atrial fibrillation ablation procedure, I determined that there was a need to complete a research study that could determine the safety and effectiveness of decreasing complaints of back pain. I researched evidence based studies and found that there was no difference in bleeding reported from femoral arterial sites when patients were allowed to have the head of their bed elevated post-procedure (after sheath pull).
Implementation:
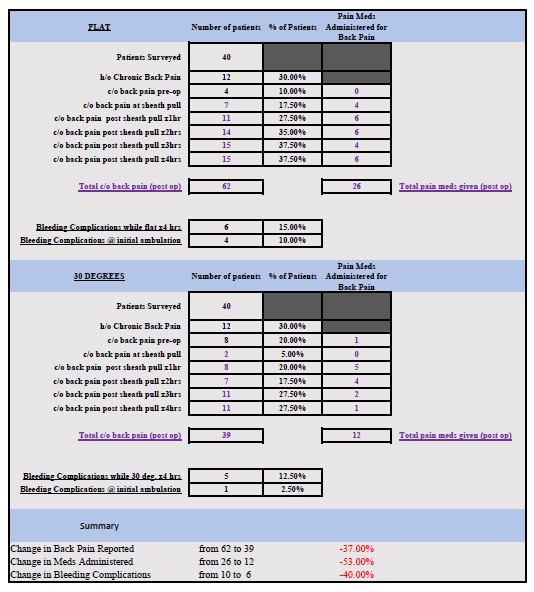
I collaborated with our management and two electrophysiology cardiologists, presented the evidence and proposed a trial for a portion of our patient population. The trial was for patients who were at VUMC for an atrial fibrillation ablation procedure, where the average length of the procedure is 3-4 hours and the patient has a “flat time” on bedrest for another 4 hours. The femoral sheaths are usually venous, so the risk of bleeding is less than a procedure where an artery is used. After meeting with management, I approached each of the other electrophysiology MDs and received approval to proceed. The protocols for changing the flat time requirement to raising the head of the bed 30 degrees were then approved by both management and electrophysiology MD’s and the request submitted through the proper channels. With the help of the RNs from our unit, we proceeded to collect data and documented the HOB elevation, medications given for back pain, bleeding issues throughout the day and bleeding upon initial ambulation.
Results:
The results showed a decrease in back pain reported by 37%. It also showed fewer meds administered for back pain by 53%. This change in procedure accomplished increased patient comfort with no increase in bleeding incidents. In fact, incidentally there was a 40% decrease in bleeding incidents compared to the group that had been kept flat after their procedure. The study was successful on multiple levels:
- Patient satisfaction expected to increase as patient discomfort and stress decrease. Expect fewer complaints about the post procedure length of time.
- Decreased cost to both the patient and VUMC for medications administered for treatment of back
- Decrease in time that RNs will spend treating back pain throughout the day.
Implications for the Future:
Opportunity to change the post procedure protocol for multiple other procedures recovered in the CCL Holding Room/ EP PACU that have potential to result in similar patient satisfaction and cost savings benefits.