The growing availability of multi-scale biomedical data sources that can be used to enable research and improve healthcare delivery has brought about what can be described as a healthcare “data age.” This new era is defined by the explosive growth in bio-molecular, clinical, and population-level data that can be readily accessed by researchers, clinicians, and decision-makers, and utilized for systems-level approaches to hypothesis generation and testing as well as operational decision-making.
However, taking full advantage of these unprecedented opportunities presents an opportunity to revisit the alignment between traditionally academic biomedical informatics (BMI) and operational healthcare information technology (HIT) personnel and activities in academic health systems. While the history of the academic field of BMI includes active engagement in the delivery of operational HIT platforms, in many contemporary settings these efforts have grown distinct.
Recent experiences during the COVID-19 pandemic have demonstrated greater coordination of BMI and HIT activities that have allowed organizations to respond to pandemic-related changes more effectively, with demonstrable and positive impact as a result. In this position paper, we discuss the challenges and opportunities associated with driving alignment between BMI and HIT, as viewed from the perspective of a learning healthcare system. In doing so, we hope to illustrate the benefits of coordination between BMI and HIT in terms of the quality, safety, and outcomes of care provided to patients and populations, demonstrating that these two groups can be “better together.”
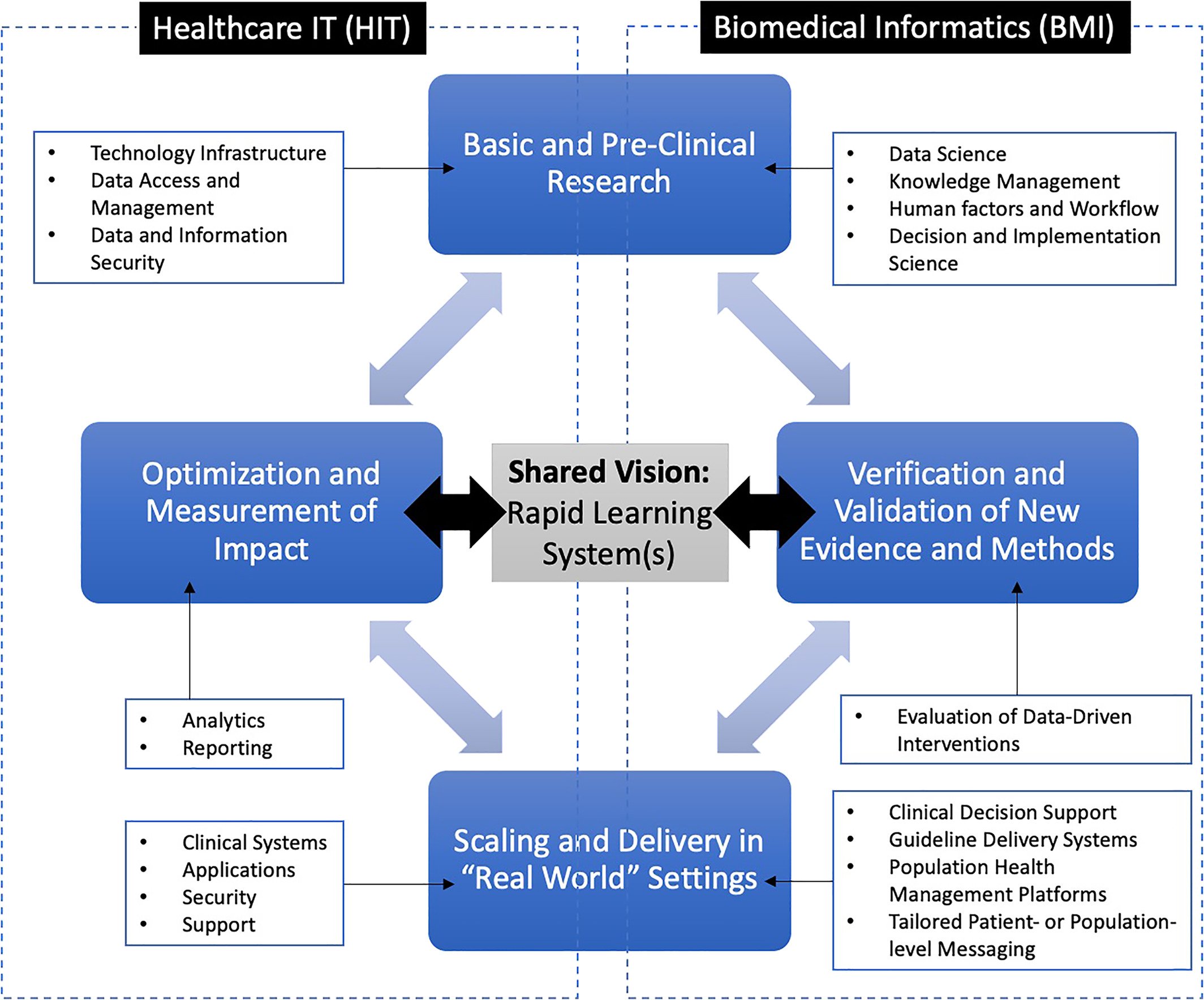
Pictured below: Conceptual model for a “rapid learning” healthcare system in which BMI and HIT work synergistically. In this example, four major stages for the design and implementation of a data-driven intervention strategy are shown, spanning the capabilities of BMI and HIT leaders and practitioners. For each stage, examples of the types of competencies and methods that contribute to each such phase are shown.
Study authors include Peter Embí, Chair of DBMI. Read the full study in Learning Health Systems here.