The diagnosis of psychosis
We are interested in the classification of schizophrenia, schizoaffective disorder and psychotic bipolar disorder. We aim to improve the reliability and validity of the available diagnoses and work towards a more personalized approach in the diagnosis and treatment of psychotic disorders.
Articles
Heckers S, Barch DM, Bustillo J, Gaebel W, Gur R, Malaspina D, Owen MJ, Schultz S, Tandon R, Tsuang M, Van Os J, Carpenter W. Structure of the psychotic disorders classification in DSM-5. Schizophrenia Research. 2013 Oct 10;150(1). 11-4.
Anxiety and psychosis
Emerging evidence shows that schizophrenia is a neurodevelopmental disorder. In other words, there are specific characteristics that can be observed in childhood in people who later develop schizophrenia. If we can identify these early characteristics, we might be able to identify children who are at high-risk and provide them with interventions to help change their developmental course. We are studying the role of inhibited temperament--an early-emerging trait characterize by fear and avoidance of new things--in risk for schizophrenia and have recently found that individuals with schizophrenia are more likely to have an inhibited temperament as children.
For more information, see: Inhibited temperament in schizophrenia
How do we study the brain in psychosis?
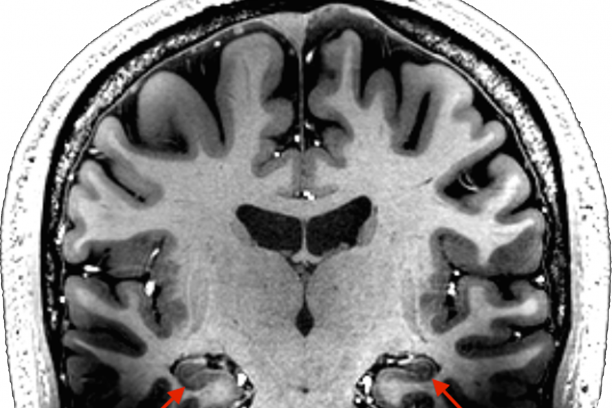
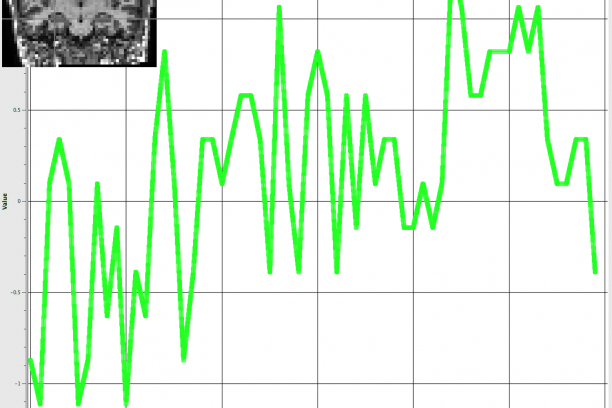
We use magnetic resonance imaging (MRI) to study the brain. MRI machines use magnetic fields to create images of the brain. MRI can be used to obtain very high-resolution images of brain structure. We also use functional MRI to study brain activity. Rather than taking one picture of the brain, with functional MRI we take quick snapshots every few seconds while a person is performing a memory task or even resting quietly. Each snapshot measures brain activity at a given moment. We can put these images together over time to look at changes in brain activity in regions such as the hippocampus. In addition to functional MRI, we collect measures of blood flow and blood volume, which enable us to examine differences in baseline brain activity.
Memory deficits in psychosis
Our ability to encode, store, and retrieve information from memory relies on the structural and functional integrity of the hippocampus. Schizophrenia is associated with impairments in memory retrieval. These cognitive impairments significantly contribute to the illness and may serve as a marker for poor prognosis or outcome. We are examining memory differences between healthy subjects and individuals with psychosis during tasks that require them to remember and use already learned relationships to make inferences about previously unpaired items. Patients with schizophrenia perform significantly worse when making judgments about the association between previously unpaired items than controls. Published data have shown that this task taps the basic cognitive processes underlying declarative memory, and may ultimately bridge human and non-human animal work investigating hippocampal memory function.
Articles
Williams LE, Avery SN, Woolard AA, Heckers S. Intact relational memory and normal hippocampal structure in the early stage of psychosis. Biological Psychiatry. 2012 Jan 1;71(2). 105-13.
Williams LE, Must A, Avery S, Woolard A, Woodward ND, Cohen NJ, Heckers S. Eye-movement behavior reveals relational memory impairment in schizophrenia. Biological Psychiatry. 2010 Oct 10;68(7). 617-24.
Hippocampal structure and function in psychosis
A major focus of the research in our lab is on the hippocampus. The hippocampus is a region of the brain important for learning, memory and emotion. Our work has shown that patients with chronic schizophrenia, but not bipolar disorder with psychosis, have a smaller hippocampus and they don’t use the hippocampus as effectively as healthy people when trying to remember events. We have also found that changes in memory, hippocampal size and function may not be present early in the illness, but instead progress over time. These studies emphasize the importance of studying patients early in psychosis. Our goal is to better understand how memory and the brain change in psychosis over time so that better treatments can be developed.
Based on this work, we have proposed that the main features of psychosis (i.e., delusions and hallucinations) originate from an abnormal interaction between the hippocampus and the cortex. Interactions between the hippocampus and cortex give rise to representations of stimuli, provided either directly by our senses or via imagery and recollection from memory. Such representations provide the basis for conscious awareness of the world and the self. The hippocampus is involved in both binding together and separating stimulus representations from one another. The core deficit of schizophrenia stems from a breakdown in how the hippocampus and cortex communicate to generate these representations. This leads to an impaired ability to classify stimulus representations as internally or externally generated (hallucinations) and to an association of stimulus features with each other, even in the absence of a true relationship (delusions).
Articles
Williams LE, Blackford JU, Luksik A, Gauthier I, Heckers S. Reduced habituation in patients with schizophrenia. Schizophrenia Research. 2013 Dec 12;151(1-3). 124-32.
Heckers S, Konradi C. Hippocampal pathology in schizophrenia. Current Topics in Behavioral Neurosciences. 4. 529-53.
Recent Publications
Talati P, Rane S, Kose S, Blackford JU, Gore J, Donahue MJ, Heckers S. Increased hippocampal CA1 cerebral blood volume in schizophrenia. Neuroimage Clinical. 2014 Jul 22;5. 359-64.
Talati P, Rane S, Kose S, Gore J, Heckers S. Anterior-posterior cerebral blood volume gradient in human subiculum. Hippocampus. 2014 May 5;24(5). 503-9.
Heckers S. Future in psychopathology research. Schizophrenia Bulletin. 2014 Mar 3;40 Suppl 2. S147-51.