Current Projects
IMPACTS (Funded by AHRQ)
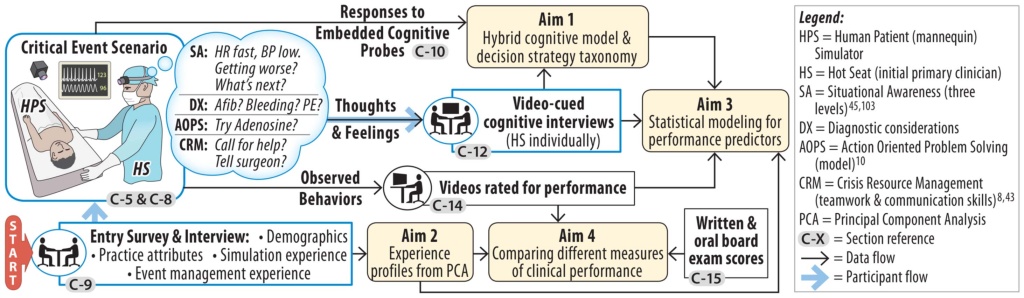
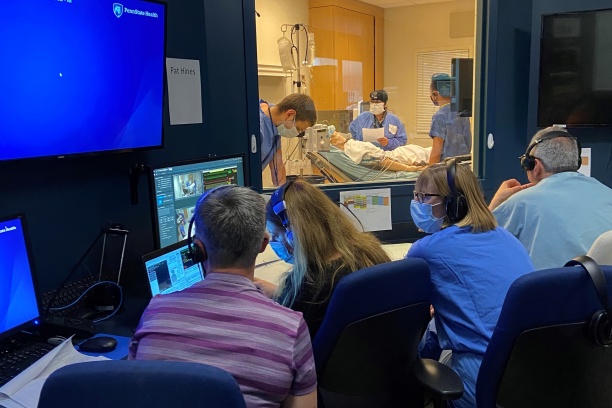
This follow up study to SARG’s first study (MOCA) seeks to go beyond measuring what is done during simulated acute patient care scenarios and study why those actions were undertaken. By using data from cognitive interviews with study participants after the simulated encounters, our primary goal is correlate the actions performed during simulated crisis events with the decision-making strategies employed to identify strategies that lead to the highest and lowest rated patient-care performances. The Specific Aims of this six-year project are to: 1) Develop and test an updated and unified cognitive model and taxonomy for clinician decision-making strategies used in critical event management; 2) Measure and describe the clinical performance of board-certified anesthesiologists managing acute perioperative events; 3) Identify general attributes of anesthesiologists (e.g., demographic variables, prior training, particularly in simulation, and practice attributes) that may influence clinical performance; and 4) Evaluate the relationship between simulation-based performance assessment and existing metrics of physicians’ competence (i.e., primary Board certification examination scores). On this project, we are collaborating closely with the American Board of Anesthesiologists (ABA).
Decision Making in Neuromuscular Blockade (Funded by Merck)
Residual neuromuscular blockade (NMB) following general anesthesia continues to be a major problem for post-surgical patients. Numerous studies demonstrate that ~40% (range 20% to 60%) of post-operative patients have residual blockade (i.e., weakness). This can cause respiratory insufficiency leading to reintubation or failure to reintubate, aspiration, and pneumonia. Neither clinical signs of motor strength (e.g., hand grip, head lift) nor qualitative twitch monitoring (i.e., visual or tactile assessment of train-of-four) are reliable indicators of adequate NMB reversal. As a result of ample scientific and clinical evidence, there is now a consensus among knowledgeable experts on the best practices for management of NMB. Yet, a substantial proportion of anesthesiologists do not follow these practices and often fail to use NMB monitors or use then incorrectly. Many fail to reverse or use inadequate doses of NMB reversal medications. We know very little about the underlying reasons and motivation for these common clinical behaviors (decisions) that deviate from evidence-based best practices. SARG is engaged in studying the ‘why’ of decision making and has developed methods to address the critical issue of better understanding decisions around NMB reversal. In this study, we are combining low-fidelity simulations (i.e., clinical vignettes) that force clinicians to make targeted decisions and surveys of clinical practice followed immediately by focused cognitive interviews to discern why they made those specific decisions.
Prior Projects
SARG-MOCA (Funded by AHRQ)
We sought to determine whether mannequin-based simulation can reliably characterize how board-certified anesthesiologists (BCAs) manage simulated medical emergencies. Our primary goal was to identify gaps in performance and to establish psychometric properties of our assessment methods. A total of 263 consenting board-certified anesthesiologists participating in simulation-based maintenance of certification in anesthesiology (MOCA) courses at one of eight simulation centers were audio-video recorded performing standardized simulated emergency scenarios. Each participated in two 20-min high-fidelity simulated medical crisis scenarios, once each as the primary anesthesiologist and the first responder. Via a Delphi technique, an independent panel of expert anesthesiologists identified critical performance elements (CPEs) for each scenario. Trained, blinded independent anesthesiologists rated the recordings using standardized rating tools. Measures included the percentage of CPEs observed and holistic (one to nine ordinal scale) ratings of participants’ technical and nontechnical (behavioral) performance. Raters also judged whether the performance was at a level expected of a BCA. Rater reliability for most measures was good. In 284 simulated emergencies, participants were rated as successfully completing 81% (interquartile range, 75 to 90%) of the CPEs. The median rating of both technical and nontechnical holistic performance was five, distributed across the nine-point scale. Approximately one-quarter of participants received low holistic ratings (i.e., ≤3). Higher-rated performances were associated with younger age but not with previous simulation experience or other individual characteristics. Calling for help was associated with better individual and team performance. Standardized simulation-based assessment identified performance gaps informing opportunities for improvement.
Project Information
If you are interested in obtaining information about or materials from the AHRQ-funded MOCA or IMPACTS studies, please contact Dr. Matthew Weinger at Matt.weinger@vumc.org.