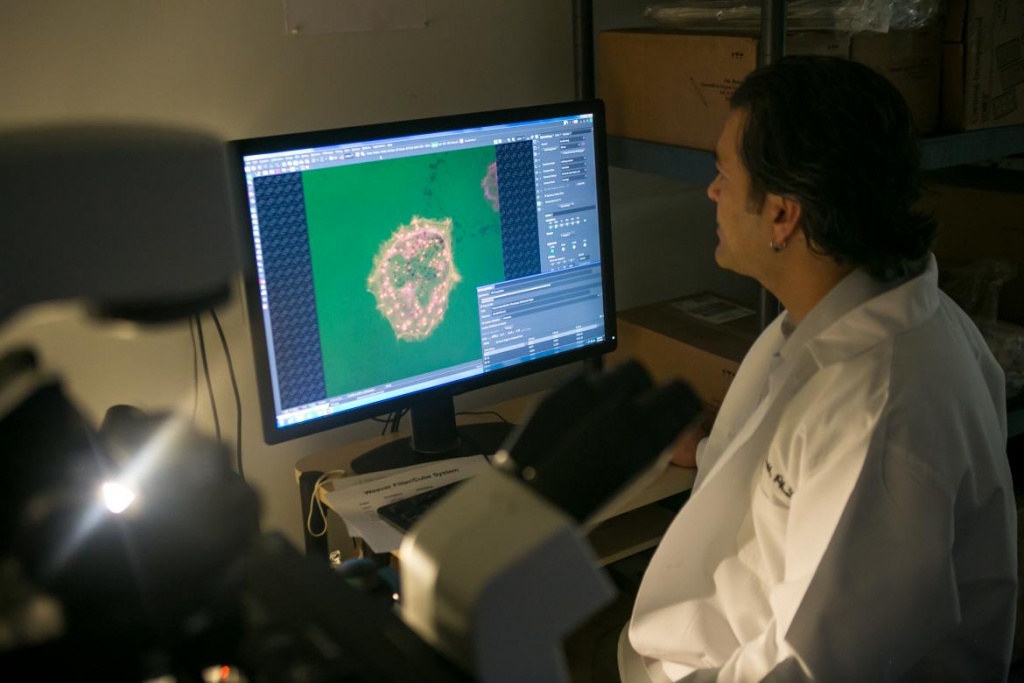
The Parekh Laboratory uses a variety of methods to understand the mechanobiology of cancer cell invasion and fibroblast activity during wound healing including microscopy (widefield, confocal, live cell, traction force), molecular and cellular techniques (RNAi, immunofluorescence, Westerns, RNAseq), and synthetic and tissue-derived scaffolds (polyacrylamide gels, polyurethanes, urinary bladder matrix):
CANCER CELL INVASION
Cancer is a leading cause of death, and long-term cancer survival rates are significantly impacted by metastases resulting from invasive cancer cell behavior. Malignant growths often present as rigid masses that are denser than surrounding normal tissue. Cancer aggressiveness is strongly associated with tissue density both clinically and in animal models, and numerous studies utilizing in vitro and in vivo extracellular matrices (ECMs) have shown that mechanical factors such as rigidity and density can regulate cancer cell invasion. The rigidity of the tumor-associated ECM promotes signaling pathways that elevate Rho-ROCK (Rho-associated kinase) activity to drive malignant behavior through increased actomyosin contractility. To penetrate cross-linked tumor and native tissues, migrating cancer cells utilize actin-rich adhesive protrusions known as invadopodia to proteolytically degrade the ECM during invasion. However, it is unclear whether rigidity signals regulate invadopodia through contractile forces or through other downstream ROCK signaling pathways. These potential mechanisms are further complicated by recent studies showing that the ROCK isoforms perform distinct functions that often have opposing effects. Therefore, ROCK may regulate invasive migration through a much more complex process than currently understood. Thus, our goal is to determine the roles of the ROCK isoforms in mediating rigidity-dependent invadopodia activity. Our proposed studies will have a profound impact on our understanding of how the mechanical properties of the tumor microenvironment regulate cancer cell invasion with implications for novel and specific anti-invasive therapies.
WOUND HEALING
Injuries resulting from accidents, diseases, and warfare are a significant health concern that result in imperfect repair and fibrosis or scar formation. The consequences of scarring can range from cosmetic abnormalities to more critical outcomes such as major body deformations and impaired function, resulting in treatments and surgeries to address both physical and psychological issues. Therefore, there exists a pressing need for new therapies that not only stimulate wound healing but manipulate this process towards a more regenerative outcome. In dermal wound healing, fibroblasts mechanosense increases in dermal wound rigidity and tension during healing and differentiate into myofibroblasts. Myofibroblasts utilize stress fibers to generate large cellular forces that excessively contract and remodel the ECM leading to scarring and fibrosis. In contrast, injured oral mucosa heals scarlessly suggesting that the intrinsic phenotype of oral mucosal fibroblasts is altered and promotes cellular contractility that facilitates regeneration. However, little information exists as to the molecular and cellular programs that define the oral mucosal fibroblast phenotype. Therefore, our long-term goal is to identify intrinsic differences in the oral mucosal fibroblast fibroblast phenotype to develop therapeutic strategies to modulate dermal fibroblast behavior in the wound bed to induce a more regenerative healing response.
PAST AND CURRENT FUNDING
American Cancer Society
National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health
National Institute of Dental and Craniofacial Research, National Institutes of Health
National Cancer Institute, National Institutes of Health
Children's Hospital of Pittsburgh Research Advisory Committee
National Organization for Hearing Research Foundation