PULMONARY ARTERIAL HYPERTENSION
Pulmonary arterial hypertension (PAH) is high blood pressure (hypertension) within the lung (pulmonary) arterial circulation. It is a disease that results in narrowing and blockage of the very smallest arteries (blood vessels) throughout the lungs. The blood vessels that are affected are about the size of a human hair. While small there are an enormous number of these vessels that in total manage nearly all of the blood that travels through the lungs. These small vessels are thus very important because nearly all of the blood in the circulation must pass through them. As these blood vessels become blocked, the pressure in the pulmonary arterial circulation increases which puts a strain on the right side of the heart. Ultimately, the pressure may increase to a point that blood cannot flow normally through the lungs. When this happens, in addition to putting a strain on the right side of the heart, blood flow to the rest of the body is inadequate.
Normal:  PAH:
PAH: 
PAH can occur in association with several other diseases such as autoimmune diseases, but often no cause is found. If PAH patients have a family history of PAH or have a mutation detected in a gene known to cause PAH, they may have heritable PAH (HPAH). If there are no other causes and no known family history, PAH is called idiopathic (IPAH). The incidence of IPAH in the general population is about 1-2 per million. The incidence of HPAH appears to be much lower.
IPAH and HPAH look virtually identical to one another in all respects. Symptoms, clinical course, and response to therapy are equal, except that HPAH may be diagnosed about 10 years earlier than IPAH. HPAH can be inherited from a male or female parent. The incidence is 2.4:1 females to males, similar to the general IPAH population. HPAH is inherited as a dominant trait, although, many persons who carry the gene do not get the disease. A gene that causes HPAH, bone morphogenetic protein receptor 2 (BMPR2) was discovered and described in 2000 by Vanderbilt University and Columbia University researchers, independently. This gene is associated with cell growth and development, as well as other cellular processes. Rare variations in the composition of this gene (also known as mutations) may lead to the formation of abnormal pulmonary arteries seen in this disease, although the precise mechanisms remain unclear. The familial form of this disease has long been an interest of the Vanderbilt group, although we do study many forms of the disease in depth including IPAH. Occasionally, patients with IPAH are found to have mutations in this gene as well, and we thus know that those patients have heritable disease that can be passed to their children (HPAH) despite no known family history of PAH.
Common symptoms of the pulmonary hypertension and reduced blood flow are passing out, shortness of breath with exercise, blue lips and fingers, and swelling of the ankles and legs. PAH can develop in men or women at any age, but is more common in women. The age of diagnosis does vary according to type. For those with HPAH and IPAH, diagnosis is most common between the ages of 20 and 40 years, although for those with many other types of PAH associated with other diseases such as autoimmune disease the age at diagnosis is 10-15 years older. PAH may progress silently for many years, and thus often takes a long time before diagnosis is made. Many patients in the early stages of PAH have mild symptoms, and believe they are just overweight, growing older, or out of shape. Even when a patient has significant symptoms, he or she may see a doctor several times before the doctor thinks about PAH, because it is an uncommon disease and many doctors will not have seen a patient who has PAH.
Exciting research in this disease at our Center has been advanced through several funding grants from the National Institutes of Health (NIH) and other funding agencies. In particular, we have a NIH grant titled “Hormonal, Metabolic, and Signaling Interaction in PAH” which began September, 2012 and will continue until July, 2017. This large program grant supports a number of human, animal model, and cell-based studies which we hope will translate into novel information and therapeutics for PAH.
HISTORY AND CURRENT STUDIES:
Our genetic studies for HPAH have been supported for the majority of the past 20 years by the National Institutes of Health. Our Vanderbilt Family Registry was initiated in 1994. The purpose of the registry is to find and enroll as many families with HPAH as possible. The more families that are enrolled the more information will become available concerning the disease. Any personal or medical data submitted is kept strictly confidential.

Our current studies: Click some of the links below to see what research we are conducting and how you might can contribute!
Carnitine Consumption and Augmentation in Pulmonary Arterial Hypertension
Interventions Against Insulin Resistance in Pulmonary Arterial Hypertension
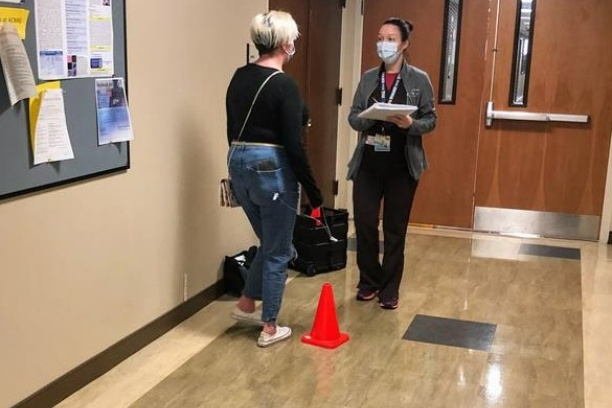
MobileHealth Intervention in PH
Risk and Resilience in Pulmonary Arterial Hypertension and Genetically Susceptible Individuals
Tamoxifen Therapy to Treat Pulmonary Arterial Hypertension (T3PAH)
Research participants are protected by a Certificate of Confidentiality from the Department of Health and Human Services. The Certificate prevents researchers from being forced to expose any information concerning subjects in their study. The major goals of the study are to understand the processes that cause the disease, attempt to develop new treatments, and provide information to patients and physicians.
For more information contact:
PULMONARY ARTERIAL HYPERTENSION STUDY
Anna Hemnes, MD Co-Director and Evan Brittain, MD Co-Director
Thomas Strayer, PhD Program Manager
P: 1-615-936-0156 FAX 1-615-322-1372
 GENETIC TESTING:
GENETIC TESTING:
How can I get genetic testing for IPAH/HPAH?
If a BMPR2 gene mutation has been identified, the research study coordinator can help you arrange genetic counseling. If you decide to be tested, the counselor will help you find a clinical laboratory that provides testing for BMPR2.
The cost of testing will vary. A blood sample from an affected relative may be needed. The accuracy of testing will usually be greater than 99%. If your family is not involved with a research group, you may wish to contact your primary care provider or a genetic counselor in your area (see the National Society of Genetic Counselors website, www.nsgc.org).
As you may be aware, this is an exciting time for genetics research in PAH and many other diseases. There are new gene discoveries being made, such that BMPR2 may not be the only gene for which screening may be appropriate, depending on the circumstance.
We can also help with determining the complex issues around gene mutations and PAH that are growing as our knowledge increases.
RESOURCES:
The Pulmonary Hypertension Association is a non-profit organization that has been pivotal in providing information for patients and physicians. They have been a wonderful partner in support of our research. Please contact them for more general information and to become involved in the fight against PAH.
 Pulmonary Hypertension Association (PHA) and the PATHLIGHT:
Pulmonary Hypertension Association (PHA) and the PATHLIGHT:
PHA is primarily a volunteer support group for patients with pulmonary hypertension of any cause. They provide education for patients and physicians about the disease. They also have a nationwide system of support groups and maintain a listing of physicians experienced with treating PAH. Contact them at following address and phone:
Pulmonary Hypertension Association
801 Roeder Road, Suite 1000
Silver Spring, MD 20910
301-565-3004
1-800-748-7274 (volunteer staffed please call in daytime)
www.phassociation.org
PHA publishes a quarterly newsletter, The PATHLIGHT, that offers many articles of interest to patients and family members. Additionally, the organization publishes a medical journal, Advances in Pulmonary Hypertension, distributed to cardiologists, pulmonologists, and rheumatologists nation-wide.
Other Resources:
 Pulmonary Arterial Hypertension KnowledgeBase: PAHKB
Pulmonary Arterial Hypertension KnowledgeBase: PAHKB
Financial:
REFERENCES:
Genetics and Mediators in pulmonary arterial hypertension. Austin ED, Loyd JE. Clinics in Chest Medicine. 2007 Mar;28(1):43-57, vii-viii. Review.
Narrative review: the enigma of pulmonary arterial hypertension: new insights from genetic studies. Newman JH, Phillips JA III, Loyd, JE, Annals of Internal Medicine. 2008 Feb 19; 148(4): 278-83. Review
What patients and their relatives think about testing for BMPR2. Jones DL, Sandberg JC, Rosenthal MJ,Saunders RC, Hannig VL, Clayton EW.J Genet Couns. 2008 Oct;17(5):452-8.
Mutation in the gene for bone morphogenetic protein receptor II as a cause of primary pulmonary hypertension in a large kindred Newman, J.H., Wheeler, L., Lane, K.B., Loyd, E., Gaddipati, R., Phillips, J.A. III, Loyd, J.E..N. Engl. J. Med. 345:319-24, 2001.
Heterozygous germline mutations in a TGF-beta receptor, BMPR2, are the cause of familial primary pulmonary hypertension. Lane, K.B., Machado, R.D., Pauciulo, M.W., Thompson, J.R., Philips, J.A. III, Loyd, J.E., Nichols, W.C., Trembath, R.C. ,Nature Genetics. 2626(1):81-84, 2000.