Stroke is the leading cause of adult disability and the third leading cause of death in the United States, affecting more than 700,000 individuals annually. Despite progress in stroke treatment, 20-30% of strokes result in death within one month and 70-80% result in significant long-term disability. Reducing stroke-related morbidity requires accurate identification of patients at highest risk for stroke and improved selection criteria for patients most likely to benefit from surgical intervention and/or medical management.
To achieve this, it is necessary to better understand the mechanisms responsible for stroke, which relate to plaque biology, vascular stenosis, flow reduction, and/or lack of collateral flow. These risk factors may act independently or in a synergistic manner. More specifically, hemodynamic compromise secondary to extracranial carotid artery occlusive disease is a well-known risk factor, and more recently it has been shown that patients with intracranial (IC) stenosis have recurrent stroke rates of 5-10% per year. However the appropriate treatment for these patients is unclear. Although angioplasty and stenting are common, the most recent prospective trial for stenting plus medical management compared to medical management alone (SAMMPRIS) was halted this year when 14% of patients treated with angioplasty combined with stenting experienced a stroke or died within the first 30 days following treatment, compared to 5.8% of patients who received medical management alone . Therefore, additional information would be useful to understand which patients stand to benefit most from different therapeutic options.
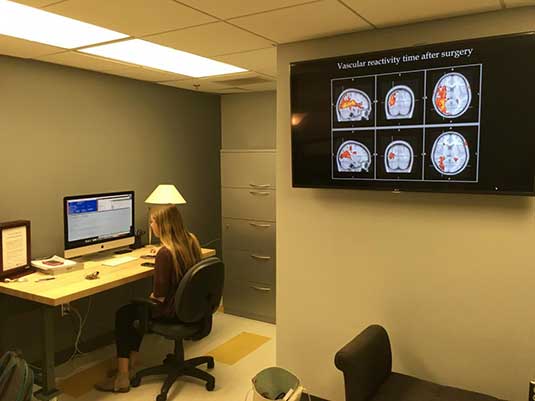
In IC stenosis patients, extensive compensatory vascular mechanisms are known to co-exist. Specifically, cerebral perfusion pressure (CPP) reductions can be compensated for by increases in parenchymal cerebral blood volume (CBV), or autoregulation. Additionally, reduced CPP can be partially or fully compensated for by a redistribution of blood, or collateral cerebral blood flow (CBF). The cerebrovascular reactivity (CVR), or the vasculature’s ability to respond to arterial hyperemia, provides an indicator of the cerebrovascular reserve, or how near the brain is to failing to meet energy demands. The presence and magnitude of collateral CBF, autoregulatory CBV and CVR have been demonstrated to correlate variably with stroke risk, however studies measuring the evolution of these parameters conjointly have not been performed.
The critical barrier to fully unraveling the relationships between the above phenomena and stroke risk, and potentially better guiding treatment decisions, lies with a lack of methodology for easily and precisely measuring these parameters. Digital subtraction angiography (DSA) is the gold standard for measuring arterial stenosis and the extent of IC collaterals, however DSA is insensitive to tissue hemodynamics. Increased oxygen extraction fraction (OEF), as measured with positron emission tomography (PET), has been shown to be an independent risk factor for subsequent stroke in patients with IC stenosis. However, few clinical centers can measure OEF, and thus OEF remains primarily a research tool. Characterization of CBF and total CBV at the tissue level is possible with perfusion computed tomography (pCT) and single photon emission computed tomography (SPECT), and reactivity can be assessed with acetazolamide challenge. These approaches have been crucial for improving diagnostic abilities, however are time-consuming and require ionizing radiation, complicating the ability to perform repeated measurements and to track changes over time and in response to therapy. Also, collateral CBF assessment requires knowledge of quantitative CBF and the vascular origin of the blood reaching the tissue, which is not possible with the above approaches.
Alternatively, magnetic resonance imaging (MRI) has been widely applied as a tool for noninvasive structural characterization of brain tissue and can be used to measure regional and global cerebral hemodynamics. The versatility of MRI has led to progress in improving diagnosis and treatment decisions for a variety of conditions. We have developed and validated specific noninvasive MRI approaches for measuring arterial CBV (aCBV) and collateral CBF using the vascular space occupancy (VASO) and vessel-specific arterial spin labeling (ASL) approaches, respectively. Furthermore, it is possible to apply the popular blood oxygen level-dependent (BOLD) MRI approach during administration of vasodilatory stimuli to assess the extent of CVR. These approaches are relatively fast and can be used conjointly to assess quantitative aCBV, collateral CBF and CVR when performed appropriately. The isolated clinical feasibility of these approaches in stroke and other neurological disorders has been established; however these approaches have not been implemented concurrently in a clinical IC stenosis protocol.
Therefore, the overall goal of this work is to implement a multi-faceted MRI exam that utilizes novel, validated, and noninvasive approaches to provide a tissue and hemodynamic signature that can be used to assess and track the relationship between large vessel disease, tissue impairment, and stroke risk in patients with IC stenosis. We anticipate that the novel approaches applied in this study will provide important clues regarding the variable hemodynamic compensation mechanisms underlying IC stenosis and stroke risk and their relevance to surgical outcomes.